Recent Posts
Most Popular
Surgeons Employ Robots To Operate On Human Retina
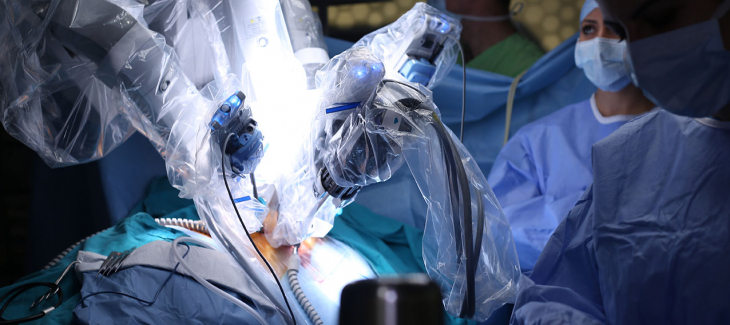
Surgery on the human eye presents a risky proposition. When robots assist the surgeon, it sounds much riskier.
In reality, though, robots are gradually taking over delicate surgeries because their precision rivals even that of an experienced surgeon.
That was certainly true earlier this year when surgeons used robots to remove fine membrane growth on the retina of six patients. These growths impair vision, and they can lead to blindness when they are left untreated.
The system, called the PRECEYES, involves a mobile arm and a joystick that controls it. Doctors can attach a variety of instruments to the machine depending on the requirements of the surgery.
Developed by a Dutch medical robotics firm, the PRECEYES is so precise it can operate in the vein of a retina, which is the size of a human hair. The membrane doctors remove using the robot is about one-tenth the width of a human hair.
The retina study involved six patients who underwent traditional surgery and six patients who underwent robotic surgery.
The traditional surgery is simple in theory. Surgeons make a tiny incision just above the pupil and insert a tiny flashlight into the 1-millimeter incision. Doctors manually remove the membrane while looking through an operating microscope.
When robots assist, the doctor inserts the tiny robot into the incision, where it separates the membrane from the retina itself.
Although the surgeries involving the robots took longer than the surgeries without them, researchers attribute that to the surgeons’ inexperience working with robots. Without robots, the surgery took one minute, 20 seconds; with robots, surgery took four minutes, 55 seconds.
Despite the slower surgery times, the robots provided precision at 10 microns in all three required directions: up/down, left/right, towards the head/towards the feet. Researchers say this level of precision is 10 times better than what surgeons can provide.
The delicate nature of the retina means that even highly skilled surgeons can cut too deeply and cause scarring or hemorrhaging, potentially leading to additional damage to the eye. The surgery is so precise that even the pulsing of blood through a surgeon’s hands can skew the cut.
Of the 12 patients involved in the study, the patients in the robot category had fewer hemorrhages and less damage to the retina.
Membrane growth on the retina causes a condition called epiretinal membrane, which can result from eye trauma or conditions such as diabetes.
The condition can also result from natural changes to the gel-like substance that fills the eye and maintains its round shape. As people age, the substance shrinks and pulls away from the retina, sometimes resulting in a tear.
The membrane is effectively a scar on the retina that obscures clear vision. In some cases, it distorts the shape of the retina. When the membrane forms over the macula, the part of the eye responsible for focusing images, the person loses the ability to read or see fine detail.
In the future, surgeons may have the capability to carry out two currently-impossible surgeries: unblocking blood vessels or injecting treatment directly into the optic nerve.
Additionally, the same technology may allow surgeons to place a fine needle under the retina and inject fluid through it for retinal gene therapy, an emerging treatment for blindness.
That process is scheduled for 2019.








Comments